Featured guests

David Nabarro is the Co-Director of the Imperial College Institute of Global Health Innovation at the Imperial College London and supports systems leadership for sustainable development through his Switzerland based social enterprise 4SD. From March 2020, Mr. Nabarro is appointed Special Envoy of WHO Director General on COVID-19.
In October 2018, he received the World Food Prize together with Lawrence Haddad for their leadership in raising the profile and building coalitions for action for better nutrition across the Sustainable Development Goals.

Clare trained in Medicine at the Universities of St. Andrews/Manchester in the UK, graduating in 1990. She was drawn to preventative and community medicine from early on and became a specialist consultant occupational physician. She also teaches communication skills.
She retired on ill-health grounds before Covid and was very ill with Covid. Experiencing ‘Long Covid’ with many other people, she noticed certain patterns of illness and the huge impact on them. She continues to raise awareness of the need for medical assessment of people with Long Covid and collaborates with patient groups on employment issues and wants to do whatever she can to keep people who have been ill with Covid to keep their jobs.
She believes in the power of communication and local communities working together in small ways to be sustainable.

Durga Sapkota, a nurse in Katmandu who continues to organize a community public health response to combat Covid-19 in Nepal. She is an ambassador for Women Deliver, a Global GoalsCast partner.
Most recently, she was elected to the board of Karma Health, an organization that is currently developing a prototype of a community-based health coverage model to ensure universal health coverage and dignified health services. As an advocate, Durga is proud to be a youth nurse advocating for women and girls to have their SRHR.

Dr. Iman Ahmed is a public health physician with over 20 years of global health experience, working at the frontline, regional and headquarters levels on humanitarian emergencies, pandemic preparedness and response (H1N1 and H5N1), noncommunicable diseases in emergencies, and COVID-19 pandemic preparedness and response with UNHCR, WHO, research institutions and governmental public health entities. During the period 2007-2010, Iman coordinated UNHCR pandemic preparedness and response for refugees, displaced communities and host populations in the Middle East and North Africa region and represented the organization at the UN System Influenza Coordination (UNSIC).
Iman is currently working as a Supervisor of COVID-19 Mass Immunization Program with the Region of Peel Public Health in Ontario, Canada. She has been part of the 4SD global health community of practice since its establishment under the leadership of Dr. David Nabarro and team in 2020.
She is a member of the Executive Committee of the Sudan Doctors Union in Canada, through which she has actively engaged in providing health diplomacy, advocacy, technical support, resource mobilization and community awareness in support of Sudan’s COVID-19 pandemic response.

John Atkinson is a designer, architect, mentor and catalyst for whole system transformation. He has instigated and led projects around the world in public and corporate settings that helped people generate fundamental change in their work and lives. He has been at the forefront of developing understanding of working with human organisations as living systems for over 25 years.

Singer-Songwriter, Guitarist, Peace Ambassador & founding Director of Dole Ndawi NGO, The Gambia. Empowering the Youth through music.
In collaboration with:
Transcript
[00:00:00] David Nabarro: People are the heart of everything that we do to deal with COVID. People are the solution, the virus is the problem.
[00:00:09] Dr. Iman Ahmed: I’m at the vaccination clinic supervising, and we’ve done a mass ramp up and it’s showing effects and I’m doing what I can, as you say.
[00:00:20] Durga Sapkota: We have counselled 550 people from 52 districts of Nepal. And uh, we have 41 nurses who are connected directly from all over the country.
[00:00:30] John Atkinson: The sort of leadership that’s needed is leadership that connects. Leadership that doesn’t seek credit for itself. Leadership that knows there’s no limit to what you can achieve if you don’t give a damn who takes the credit.
[00:00:43] David Nabarro: It’s time to do everything possible to increase the space that enables the G7 leaders to understand that it’s okay to lead for the world.
[00:00:56] Claudia Romo Edelman: Welcome to the Global GoalsCast.
[00:01:05] Edie Lush: The podcast that explores how we can change the world.
[00:01:08] Claudia Romo Edelman: In this episode, making the world COVID ready.
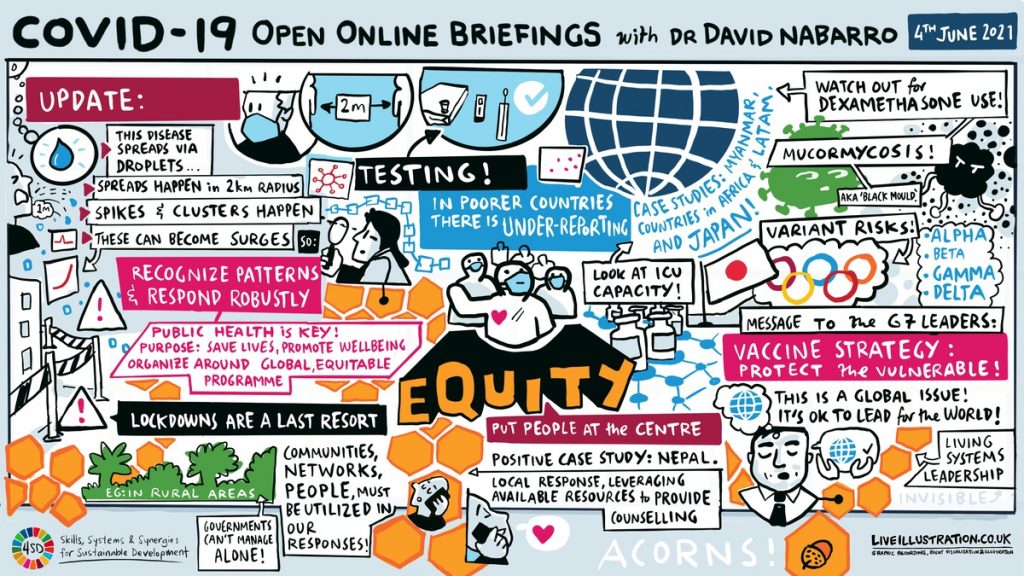
[00:01:12] Edie Lush: The Corona virus is here to stay and we have to learn to live with it in a way that keeps us all safe. Don’t just wait around for vaccines, understand the disease and how it’s spread. Recognize the patterns and block them.
[00:01:27] Claudia Romo Edelman: I get it, respect the virus, but never let it rule us.
[00:01:35] Nazeem: Keep on going, going, going, moving, shaking. Keep them positive vibes, vibes, vibes.
[00:01:46] Edie Lush: That’s Gambian singer Nazeem with his anthem, COVID ready.
[00:01:50] Claudia Romo Edelman: Important message. COVID ready. And learning to live with COVID-19 is also how we learn to be ready for future pathogens, which we know Edie, that will come in a moment. We will hear a global update on the pandemic and what it will take to be COVID ready.
[00:02:09] Edie Lush: Spoiler alert! It will take a new kind of leadership. Both leadership from rich countries on behalf of the entire world and grassroots leadership everywhere to curb the virus and keep people safe.
[00:02:23] Claudia Romo Edelman: All right. All that right after this message.
[00:02:29] Michelle: This episode of Global GoalsCast is brought to you by our listeners.
That’s right. Listeners like you who care about the future, please spread the word. Tell your friends about Global GoalsCast. Hit the like and subscribe and give us five stars. Thanks also to CBS News Digital and Universal Production Music.
[00:02:53] Claudia Romo Edelman: Welcome back. I’m Claudia Romo Edelman.
[00:02:56] Edie Lush: And I am Edie Lush. The pandemic is not over. We’ve said that before, but we are repeating it today so we can focus on what truly needs to be done.
[00:03:07] Claudia Romo Edelman: That’s right Edie. In fact, we are going from a pandemic disease to an endemic one, a virus that will always be there as a threat.
[00:03:19] Edie Lush: Vaccines are great, but there is not enough vaccine and it isn’t spread equitably. So COVID is continuing to spread particularly in poor communities.
[00:03:30] Claudia Romo Edelman: And it will continue to spread unless we adapt both globally and locally.
[00:03:36] Edie Lush: But we can do this because after 16 months we know a lot about the patterns that the virus follows.
If we focus on those patterns, we can curve the virus, even without enough vaccine.
[00:03:48] Claudia Romo Edelman: And to understand this more deeply, we joined the regular briefing by Dr. David Nabarro, the special Envoy of the World Health Organization, my former boss, and a very dear friend of Global GoalsCast.
[00:04:02] Edie Lush: Claudia these briefings are so powerful. In this session, he offered some blunt advice on what the rich world must do to protect everyone. And he introduced us to three women who have been working hard to support their communities through the pandemic.
[00:04:18] Claudia Romo Edelman: Dr. Nabarro began with a summary of how much we know now about how the virus spread.
[00:04:25] David Nabarro: The virus is almost entirely transmitted through droplets.
That means that you could get the virus if you’re within two meters of an infected person and you are not, in any way, protected from inhaling the virus that they have either coughed out or spluttered out or breathed out in their respiratory secretions. But that two meters is quite important. Although there are occasional accounts of the virus being airborne, which means it can be transported quite long distances, several meters by gusts of air.
The majority of transmission is these droplets, which are quite heavy and which sink to the ground within about a meter of people’s mouths. So that means that when the disease spreads, it spreads in a very localized way. Usually what happens is you get clusters of transmission that appear, and they then turn into spikes of cases and perhaps in a diameter of about one kilometer or more, you might end up with lots of people with the disease, perhaps a hundred or so, but then outside that one kilometer diameter, the numbers are much, much lower. So this explains why quite often, when people are describing what COVID feels like in a community, they talk about a situation that is incredibly patchy.
But I’m asking people to look underneath the numbers, to look at the pattern of disease, to look where there may be clusters developing, where there are signs that there’s a spike emerging. And then where that spike of disease might be turning into an explosive surge. Which is then associated with a lot of suffering and death, like we’ve seen in some of the countries around the world recently.
So, if the pattern is you start with a small cluster, it turns into a spike which may turn into a surge and then be an explosive outbreak, quite obviously the strategy has to be recognize your pattern, respond rapidly and robustly in order to stop things from deteriorating. And the quicker and more robust your response at the beginning of the arrival of the virus in a community, the less virus gets circulated and the easier the job of containing the outbreak is. The more you wait, whether it’s deliberately or by accident, the more likely it is that there’s going to be a lot of virus, the more likely it is that sooner or later an explosive outbreak will develop and the harder it will be to deal with it.
[00:07:39] Edie Lush: So you have to get deep into communities everywhere in the world.
[00:07:44] David Nabarro: We’ve said in the World Health Organization, that if you want to reduce spread, you have to restrict the number of times people contact others. You want to reduce the opportunities for the virus to spread. And at the same time you would like people to behave in ways that also make it less likely for the virus to spread.
How do you reduce opportunities? You encourage people to stop meeting each other. How do you reduce the numbers of times people meet with others? You require them to stay still. What do you do if you’re really worried because you’ve got a lot of cases building up? You impose something called a lockdown. The kind of measure that was introduced when there’s a jail break, you just stop everybody moving. And it’s a very powerful method, but lockdowns should really only be used as the last resort in dealing with this pandemic. They should be used when the situation is extremely serious, because the trouble with a lockdown is it has terrible collateral impact. Poor people in particular find it really hard to keep earning. Especially if they’re on daily wages, people living in confined, confined, living conditions, they find it very hard to be able to isolate and manage themselves when they’ve been locked down. And so what I’m going to say is that the pathway to the future with this pandemic is to recognize the patterns of disease and to get ready to deal with them.
Right at the center of the response is people and people are at the heart of everything that we do to deal with COVID. People’s behavior reduces spread, and also people’s behavior determines whether or not they’re able to get early treatment and to survive as a result of the disease. People are the solution. The virus is the problem.
And then to enable people to do their work effectively, public health is essential. Public health in order to help detect the early cases, to pick up the spikes, to prevent them from becoming surges, to enable people to not transmit the virus to each other. And that means you’ve got to be on the alert, you got to be able to test people when they’ve got symptoms, and you’ve got to be able to help people to isolate, to isolate as long as they are infectious. If people won’t isolate, then, I’m afraid, you’ve got a problem. And people won’t isolate if they feel they’re going to lose out financially or in terms of any other attribute that they have, that’s precious to them and they don’t want to lose.
Then they won’t isolate. And we know from all sorts of data over the last few months that if folk do not isolate, then the virus will go on spreading. So public health is key. And it’s not sophisticated stuff, that’s not lots of hospitals. That’s having local neighborhood health workers who keep an eye on their communities.
If Durga Sapkota, who is connecting with us, I believe from Nepal would like to just tell us a bit about what’s happening in her community.
[00:11:33] Durga Sapkota: Thank you so much, Dr. David, I really feel really honored and thrilled to be part of this discussion again.
[00:11:40] Edie Lush: Durga is a nurse in Katmandu and she’s an ambassador for Women Deliver, one of our Global GoalsCast partners. She’s also the embodiment of Dr. Nabarro’s point. Blocking the virus requires grassroots intervention. Durga’s story broke our hearts and inspired us too.
[00:11:57] Durga Sapkota: I lost my mother at the starting of the first wave. And it took around eight, nine months, except the fact that she’s no more with us. Grieving period was very, very long. And the stigma we faced and I don’t have any words to express all the sufferings and all the fear and the trauma.
At the starting of the second wave, we lost our grandmother-in-law. And being the healthcare provider, I was the one to take care of my family. And one of whom the family members ultimately refer to when it comes in managing the health.
[00:12:37] David Nabarro: Those of you who live in Europe or in North America are used to being able to call for an ambulance and it comes sooner or later. And then you get looked after and you will get to a hospital, again, sooner or later. But I just tell you in Katmandu, firstly, ambulances don’t always come because the roads often are not quite good.
And then secondly, the hospitals are super hard to get into. And if you don’t have cash, it can be very, very hard to get the treatment you need. For the staff it’s rotten difficult. They face a lot of physical abuse and they’re often short of equipment. It’s just the reality of being in a poor place.
[00:13:31] Durga Sapkota: I had witnessed the knowledge and information gaps related to the COVID very precisely. And with the beginning of the second wave, like the health system was extremely overstressed and mortality was very high irrespective of their group, lots of misinformation and this information related to COVID was there everywhere in the family, community, and media. And like pursuing my master’s degree in nursing. And I realized that the students like me who are studying master’s degree, bachelor degree and the teachers, and also the people that are searching for the jobs have the knowledge and the skills required to break the chain of infection in the community. But they are not part of the formal curative health system.
[00:14:18] Edie Lush: Having lost so much herself, Durga understood the crisis and stepped in.
[00:14:26] Durga Sapkota: We created a network called COVID special nurses group to work in the prevention of COVID infection and the promotion of health. And so we did the piloting of the three days to understand what kind of problems people are facing while staying at home isolation, and what kinds of help and information do the people need.
So in three days we counseled around 75 people from 32 districts and made a, uh, health model for telehealth counseling. And we provide counseling from the prevent and promotive part and as for need, we have been providing special services like we do free consultation service that is psychological and psychiatric consultation.
And many more from the experts, healthcare professionals. We also facilitate first sourcing hospital beds and managing oxygen to do as we have been discharged from the hospital with the oxygen requirements. Also we have been managing the ambulances and also we provide action related information and many more.
We have collaborated with the ministry of health and work in the core team member to make home isolation booklet for the community people. And also recently we provided online training to four batches of school, health nurses who are working at the community isolation centres, which was organized by a nursing and social psychology devision, and also recognizing the important of mental health issues, especially at the front liners. We have been organizing a stress management session, for the frontliners by the nurses who had been specializing in the psychiatric nursing. And by now, we have councelled 550 people from 52 districts of Nepal. And we have 41 nurses who are connected directly from all over the country in Distinga Stadium. And at last I would like to say that we have been doing this as a part of the volunteering activities, yeah.
Thank you so much Dr. David.
[00:16:30] David Nabarro: That is the most wonderful story of an initiative by one person following a terrible bereavement to actually try to support people who really are feeling helpless. And that story you just heard from Durga is very special. I’m not going to say that it’s typical because each story is its own story. But it’s somebody like Durga just saying I’m going to help.
[00:17:06] Edie Lush: I found that really moving and so instructive of what it takes. Next we’ll hear another story from a very different country, yet a very similar message. Help comes at the local level and builds one person at a time, but it isn’t always easy. Even in the rich world as occupational health physician Clare Rayner. who’s been battling with long COVID explains.
[00:17:29] David Nabarro: And we must never forget that one in 10 people who get COVID have an illness that lingers and makes them pretty miserable.
Clare, I’m not so much interested in your personal experiences, though of course, they’re always in my heart, but I am interested in how much you feel you’re getting through that long COVID must be taken seriously.
[00:17:55] Clare Rayner: Not at all. I really sad to say. We’re 14 or 15 months in and a lot of the people, in fact, in the first wave for us still struggling to access any sort of medical assessment in the UK.
People have not had the most basic of medical assessments at all up to 15 months where some of them now are being assessed. We’re finding very significant levels of heart damage and scarring, things that could have been treated earlier, like pericarditis. The brain effects and very, very worryingly blood clots in the brain that have probably been chronic and been there since the beginning, and these are only being discovered now people are starting to look, but people are pretty desperate. The other thing is, is the impact on employment. People are losing their jobs left, right and center because they’ve been off for this length of time. I get really upset talking about actually, because I think just, you know, the importance of employment is so close to my heart, but I want to tell one little story of an acorn, which has grown because sometimes I get discouraged.
I’ve been trying to help people to have dialogue with their employers. And so I wrote a little leaflets a while back on what people could ask for in discussion with employers. I had one of my friends, a non-medical friend who is an English graduate translate what I wrote into very straightforward language.
And we’ve just now engaging with unions and particularly and with employers, and we’ve engaged something called the society of occupational medicine.
Anyway, that has grown and grown and it’s been nationally accepted. From that tiny acorn of writing a little leaflet to try and facilitate conversation with people and retain that jobs.
This week, I found that the European countries want to translate it into 20 languages.
[00:19:49] David Nabarro: Acorns, acorns. You’re all planting acorns, Claire, you are so welcome here. Come as often as you can. We love you having you here. And you and the group of long COVID suffers who’ve been joining us, I think have had a massive impact.
[00:20:09] Edie Lush: As Dr. Nabarro is about to wrap up the briefing, he looked over the Zoom gallery and spotted a familiar face, or at least part of a familiar face. Iman Ahmed, a health colleague who works with the Sudanese diaspora in Canada.
[00:20:22] David Nabarro: Iman, you’re wearing a beautiful thing. Are you, are you on due or something? Where are you?
[00:20:27] Dr. Iman Ahmed: So I’m at the vaccination clinic and, uh, supervising and we’ve done a mass ramp up and, and it it’s showing effects. So at least at our smaller level, in the region of scale.
[00:20:44] David Nabarro: Oh I see.
[00:20:44] Dr. Iman Ahmed: And I’m doing what I can, as you say.
[00:20:47] David Nabarro: Keep masked, keep masked. I like to see that you got the double technique on. Very good.
[00:20:52] Dr. Iman Ahmed: Thank you. Thank you.
[00:20:57] David Nabarro: So all our speakers today. Thank you so much for speaking from your heart and for sharing and in particular for giving us these stories of hope, amidst some of the tragedy that so many have experienced.
[00:21:15] Edie Lush: Community action is crucial, but Dr. Navarro made it clear. It needs to be accompanied by a new attitude from the rich world.
[00:21:25] David Nabarro: And the core question is, do we treat the pandemic differently in countries that can afford to buy up a lot of vaccine, to immunize a lot of their population and therefore intend to use vaccination as the primary means of containing and ending the pandemic.
And given this gas supplies, vaccines, is it morally, economically and in public health terms, right? That wealthy nations should be purchasing and then reserving, and then holding in stock, large amounts of vaccine, even to permit their populations, to have a booster dose, if necessary towards the end of this year, when the actual access to vaccine in poor countries is extremely small. And we know that in poor countries, an awful lot of people are dying who would, if they’d been vaccinated, not die. And is it right? That, that is the way in which world vaccines are being distributed. The only people who can decide that it’s not right and act on it are the leaders of nations, because we don’t have a world government. We don’t have an authority in the world that can actually require governments to do things different. So we will only move to a universal recognition that for now the correct vaccine strategy is one of protecting the vulnerable everywhere.
We’ll only move there if the leaders of individual nations will come together and agree that that’s what they want to do. Now in our world today, we have a number of nations that are more powerful than others. So I actually think we will only get there if the leaders of the G7 nations can actually start to look at each other in the eye and say, we are responsible for helping the people of the world move through this pandemic as the virus starts to become endemic in our societies. And only the G7 leaders will be able to help us find a way through this if we’re going to do it as a world and do it together. Yes. They then can embrace the G20 leaders who are the next circle of economically powerful leaders and bring them on board and I’m absolutely certain that they will breathe a huge sigh of relief.
But most importantly, the leaders of the developing nations are absolutely desperate for the G7 leaders to start treating this pandemic as a global issue. It’s time to do everything possible to increase the space that enables the G7 leaders to understand that it’s okay to lead for the world.
It’s okay to lead for the people of your world. You are actually serving your constituents better if you lead for the world, then if you just create your jurisdiction for your leadership as being just the citizens who were eligible to vote for you and their families. No. Leadership of powerful nations in the world today, I believe, has to be about leading for the world.
[00:25:15] Edie Lush: This episode of Global GoalsCast comes down to one thought. Leadership. Dr. Nabarro asked colleague Jonathan Atkinson to sum up.
[00:25:24] John Atkinson: So people focus on vaccines, or they focus on testing, or they focus on travel restrictions or on mask wearing. And all of these things are important. But what we’ve heard today really, or what I think I’ve heard is a lot of stories of people who’ve just got on with doing what they can do, not knowing, or necessarily looking for, you know, how far this can go. Just, this is the right thing to happen and the sort of leadership that’s needed at this point for us, we’ve called it systems leadership, David, over this time is leadership that connects. Leadership that doesn’t speak credit for itself. Leadership that knows there’s no limit to what you can achieve if you don’t give a damn who takes the credit. So it’s leadership that says let’s devolve by default, let’s see our role as removing the obstacles that stop people just getting on with doing good things, and whether that’s how they connect to other people, whether that’s how they connect to information, whether that’s how they connect to resources, doesn’t matter.
And it needs to take place in every single one of us. It needs to take place in the sort of local activity that we’ve seen and we’ve heard described today, whether that’s by municipalities or whether it’s by individuals or whether it’s by health professionals, it needs to take place within public health, it needs to take place at government level and it needs to take place internationally.
But it’s all about really establishing how are we in relationship with each other about these things that we need to do so that people can just get on and do more of the right things more at the right time, more of the time because they choose to.
[00:27:00] David Nabarro: And I just want to tell you all that the kind of leadership that John and Holly who’s also here and others have been encouraging is a leadership that actually gets extraordinary results. But with the leaders themselves almost always being barely visible. Isn’t that right, John? It’s invisible leadership is what he wants.
[00:27:27] John Atkinson: It’s absolutely right. If it becomes about you and your ego, you lose people’s commitment to make it happen. It’s got to be about an act of generosity and an act of care.
[00:27:38] David Nabarro: And there’s plenty of it around, you’ve heard examples today, and there are many more examples in society. And the great thing about this form of leadership, because it’s invisible, is that an awful lot of folk just don’t realize it’s happening, but it’s the magic that keeps human societies going. Without that, we wouldn’t be anything like what we are as a race today. And we just have to keep finding it because it’s a bit out of fashion at the moment, but we will get it back into fashion as quick as we can.
[00:28:20] Edie Lush: Claudia, I think I can hear it raining in New York and it’s raining here in London. The joys of recording from the home studio.
Claudia that point about invisible leadership, I really love it. Leadership without credit or ego. In David’s briefing. He used the analogy of the honeycomb, each person taking an action by themselves that could help others.
I think the jargony way to say it might be a network effect. And the people on David’s call aren’t necessarily famous. They’re nurses, public health officials, doing something that they know is important, but of course, sometimes it does help to be already famous. And Claudia I know that you personally worked with a lot of celebrities during your time at UNHCR, and I’d love to hear how you think celebrity can sometimes help shine a light on great work that’s being done by some of these more invisible heroes.
[00:29:20] Claudia Romo Edelman: Systemic change is hard and the challenges that the world faces many times. Need a lot of people supporting decisions that have to happen. So celebrities can be helpful in a number of ways, one is opening doors when they are closed.
For example, Bono and the work that we’ve done in public health. He was instrumental not only in bringing his fans in through his concerts and his messages, but also. Calling up presidents of countries that they don’t necessarily want to take the phone call of a non-for-profit organization, like the global fund to fight aids, tuberculosis and malaria, or Angelina Jolie, really winning the hearts and minds of millions of people that were her fans to understand what it means to be a refugee.
And I think that the leaders of the G7 countries that are meeting in a couple of days from now have to feel that the work of those invisible heroes is seen by others. They need to feel that people care about our world in which we all will be safer when we all are safe and the vaccine distribution will matter.
And I think that the more we can mobilize everything that is there to mobilize so that political leaders of the G7 can feel the love and can feel the pressure, it’s instrumental.
[00:30:43] Edie Lush: And I think this idea about global cooperation. If we can build it around vaccine equity could help the world advance further in being COVID ready. For example, I was in Saudi Arabia again last week, Claudia, and I was mc-ing an event which was talking about travel and tourism recovery. So I had 14 ministers of tourism all on stage talking about how important it was to have international visitors back to their country to get their economies going again.
The tourism minister of Greece saying that by the end of June, he was going to have all of his islands, all the people who lived on those islands vaccinated in order to welcome the world, that minister of tourism for Iraq saying how important it was for him to get his country going, now that ISIS has gone.
And he said something about how tourism is so important to bring cultures and communities together. And at the moment, it is totally globally uncoordinated. The test and trace system in every country is different. The apps you have to download in order to just move around safely, completely different. We can’t have a situation where going to Portugal is different to going to Greece is different to going Jamaica, which is different to going to the Maldives.
It doesn’t work now. So if we can build some kind of solidarity in response to getting the vaccine equitably distributed, I would like to build a case that we can also work together to get the rest of the economy and travel tourism also coordinated because that will help us build back stronger together.
[00:32:39] Claudia Romo Edelman: It’s so interesting that you mentioned travel. I didn’t actually register that, but if we learn something today is that we need the world to get COVID ready. This is here to stay. Global coordination will be essential in so many aspects, whether it’s travel, schooling, everything will have to actually have an impact on coordination, but we need global solidarity.
And there’s a huge opportunity Edie, for leaders to be trusted again. And look, it just started talking about trust and started raining here because this is really one area where political leaders have lost the trust battle with people. After COVID people distrust their governments of being able and capable, not only to deal with the pandemic, but also to be generous to each other.
[00:33:31] Edie Lush: So we don’t have all the answers, but we are going to keep listening or can they keep bringing you these briefings? And we’ll keep talking.
[00:33:42] Claudia Romo Edelman: And Edie, as every week we’re bringing our audience, the three facts and three actions that they can take and they can use to show off with their mother-in-laws about how much they know about this pandemic.
[00:33:55] Edie Lush: So let’s have the three facts! Fact number one. Testing rates in high income countries are a hundred times the rates in low-income countries, and that is contributing to unmonitored an uncontrolled spread of the virus.
[00:34:10] Claudia Romo Edelman: Fact number two.High income countries have administered nearly 100 times more vaccine doses per inhabitant, than low-income countries leaving millions of healthcare workers and vulnerable populations unprotected in the world’s poorest countries.
[00:34:28] Edie Lush: And, fact number three. Health workers in many countries are still unprotected due to a lack of PPE.
So three actions you can take, Claudia.
[00:34:42] Claudia Romo Edelman: Action number one, use your voice. The G7 leaders happening in a couple of days. They care about what people are saying about voters and taxpayers. Send a letter to your Senator, send a letter to your government. And otherwise, use your social media. The G7 matters. Use your voice to let them know you’re paying attention, and yet you want a vaccine distribution that is fair for the world.
[00:35:07] Edie Lush: Action number two. Support organizations and people that are doing great work and get involved yourself. The good Sam responders app in the UK allows you to do shopping for a neighbor who might need it, go to a pharmacy to pick up a prescription, or just be a voice on the end of the phone to somebody who has COVID and needs to chat.
You can search out the similar app in your country and get involved yourself.
[00:35:33] Claudia Romo Edelman: Action. Drop the mic. Shout out to someone who’s an invisible worker, making invisible heroes, visible champions.
[00:35:42] Edie Lush: That is a wrap. Claudia, my message to you is that global solidarity against COVID-19 is not just the right thing to do. It’s the fastest and most effective way to defeat the pandemic and get all our lives and economies back to normal.
[00:35:57] Claudia Romo Edelman: And we’re making a commitment to everyone in the audience to keep you up to date about the things that we need to be ready and aware in this, getting the world COVID ready, moving forward.
I just want to say goodbye and thank you. Thank you all for listening. Thank you, Dr. David Nabarro and all his wonderful team. Thank you for the Global GoalsCast team. And we see you very soon. Thank you so much. Bye-bye!
[00:36:25] Edie Lush: Bye! Remember to like, subscribe, leave a comment telling us how much you enjoyed this episode.
[00:36:35] Michelle: Global GoalsCast was hosted by Edie Lush and Claudia Romo Edelman. We are editorial gurued by Mike Oreskes. Editing and sound production by Simon James. Our operations director is Michelle Cooperider.
Music in this episode was courtesy of Universal Production Music. One of the world’s leading production music companies, creating and licensing music for film, television, advertising, broadcast, and other media, including podcasts.
Original music by Neil Hale, Angelica Garcia, Simon James, Katie Krone and Andrew Phillips. Thanks also to CBS News Digital.